The COVID Mothers Study: How ABM’s Worldwide Network of Physicians Collaborated on Urgent Research
By Melissa Bartick, MD, MS, FABM
This week, the results of the COVID Mothers Study were published in Breastfeeding Medicine, providing more evidence that it may be safe to keep mothers and newborns together and, importantly, that separating them causes significant harm. Indeed, as the authors point out, the “significantly low rate of [neonatal] hospitalization in the literature indicates it may be nearly impossible to demonstrate a clinical benefit from disrupting Baby-Friendly practices.”
Like other studies involving COVID-19, coordinating and launching this study had to be done quickly, for answers were urgently needed. As the World Health Organization declared a pandemic on March 11, news stories appeared about infected mothers being forcibly separated from their infants with the rationale of protecting infants from infection, without evidence to support this practice, which violated existing quality standards of maternity care from the World Health Organization. By the end of March, I, together with Dr. Lori Feldman-Winter, and Dr. Verónica Valdés had planned to gather such evidence. Lori and I had known one another for many years and had collaborated before, and we both met Verónica when she volunteered to help us after I sent out an email to the ABM membership. Lori and I are Americans; Verónica is Chilean. We met and planned out a study using a survey, initially thinking we would quickly and easily get a large number of respondents by recruiting from social media platforms. Lori was also able to recruit statistical support (Dr. John Gaughan, PhD) and medical student manpower with social media expertise (Nikhil Bhana, B.S.) from her university.
We took full advantage of ABM’s internal communications networks to help us line up people who could translate and distribute the survey. Word of the study spread around the world. Having heard of the study through an Italian ABM member, we were thrilled to be approached by Angela Giusti, PhD of the Italian National Institute of Health (ISS) and Elise Chapin, MEd of the Italian National Committee for UNICEF, and they joined our team. Not long afterward, Dr. Maite Hernández-Aguilar, an ABM member, joined us and became instrumental in getting the survey around Spain, where cases numbers were very high. Other ABM members in Germany (Dr. Elien Rouw) and Saudi Arabia (Dr. Fouzia AlHreashy) came forward, and still other members led us to contacts that helped with translation and recruitment in Brazil and other parts of Latin America, as well as Asia. This is how we came to meet nursing professor Elysângela Dittz Duarte, RN, PhD of Brazil, an important member of the research team.
When it became clear that there were not nearly as many birthing women with histories of active COVID as the news led us to believe, we relied on our networks of doctors and their colleagues, including midwives and other health professionals, to get the survey to patients they knew. We engaged Lucia Jenkins, RN, IBCLC of Baby Café USA to send the survey out immediately via social media to her network of 158 breastfeeding support sites in 28 U.S. States, expanding geographical reach. We are able to engage many American ABM members, including those who worked in COVID “hot spots,” to directly reach their patients. Together, our total sample size of 357 infants is one of the largest to date for a single study, and the neonatal subset of 129 infants, with 84 SARS-CoV-2+ mothers, is among one of the larger sizes for a COVID study.
We could not have done this study without the amazing network that ABM provided, as well as many other people we knew or got to know around the world. We are grateful to all of them, and to the mothers who took the time to answer our survey.
ABM Candid Conversations: A Virtual Interview with Protocol Authors Helen Johnson, MD and Katrina Mitchell, MD IBCLC
ABM is excited to launch the beginning of our Candid Conversations series, featuring ABM members and their various initiatives within the Academy as well as their professional lives. This week, ABM sat down virtually with Helen Johnson, MD and Katrina Mitchell, MD IBCLC, two authors of our most recent protocol Breast Cancer and Breastfeeding, to discuss how they became interested in breastfeeding medicine, what lead them to creating their protocol, and what shifts they’ve seen in practice over the last year with the current health crisis.

Katrina Mitchell, MD IBCLC 
Helen Johnson, MD
Q: Please introduce yourself and provide any background or work information you’d like shared.
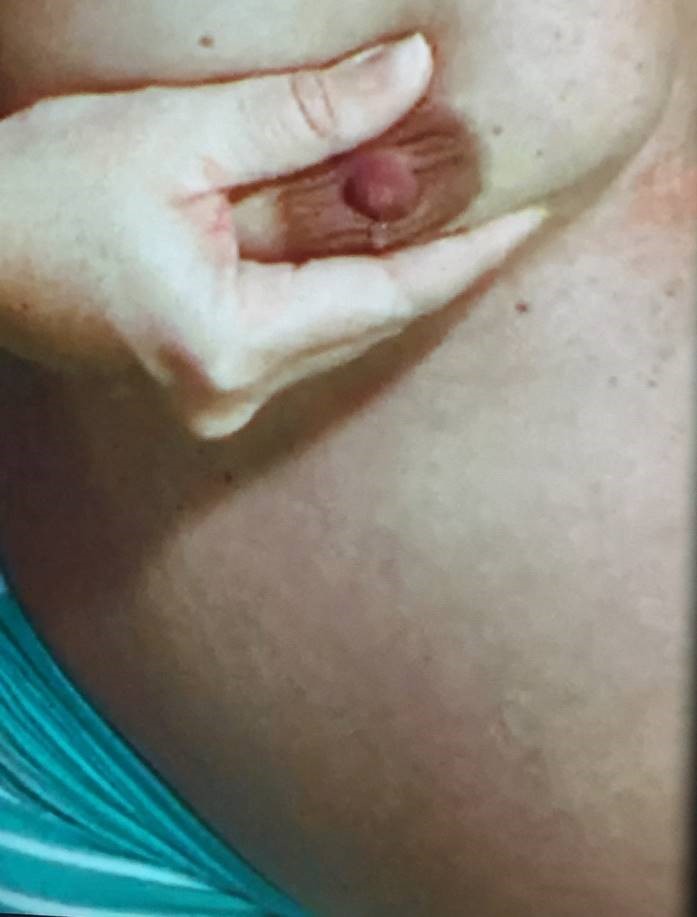
HJ: I am a native of Tampa, Florida and a graduate of Brown University’s Program in Liberal Medical Education. I am currently in my fourth year of general surgery residency at East Carolina University/Vidant Medical Center in Greenville, North Carolina. After residency I plan to pursue fellowship training in breast surgical oncology, and am currently working towards IBCLC certification. My goal is to be able to provide high-quality care for patients with any breast condition, whether benign or malignant, and/or occurring during unique periods such as pregnancy or lactation. I am passionate about research and evidence-based medicine, and hope to contribute to the advancement of scientific and medical knowledge related to breast disease.
KM: I’m a breast surgeon and lactation consultant in Santa Barbara, California. My practice focuses on the operative management of breast cancer, but I also care for breastfeeding dyads with a variety of lactation-related questions and concerns.
Q: How did you discover/enter the world of breastfeeding medicine?
HJ: I experienced challenges breastfeeding my children. When I sought medical evaluation for a breast condition, I was shocked by the fragmentation of care. I was able to receive timely, helpful support from a lactation consultant, but it was much more difficult to find a clinician with prescribing privileges who was knowledgeable about lactation. A colleague encouraged me to join the Facebook group Doctor Mothers Interested in Lactation Knowledge (“Dr MILK”), where I learned a great deal about breastfeeding from other physicians. It was through Dr MILK that I first learned about ABM and the field of breastfeeding medicine. I was so pleased to learn that there is a field devoted to breastfeeding medicine including care of the lactating breast, as I want to be able to help any patient with any breast concern.
KM: During my breast surgical oncology fellowship in Houston, Pamela Berens was my breastfeeding medicine physician after the birth of my son. She introduced me to the ABM, and my son and I attended our first conference in Portugal when he was 7 months old.
Q: How has being a member of ABM contributed towards your profession/life?
HJ: Contributing to ABM protocols has been such a rewarding experience. I have gained a deeper appreciation for the strength of the evidence for specific recommendations, and the process of developing societal guidelines. I have especially enjoyed collaborating with other physicians who are passionate about breastfeeding medicine. Through these collaborations, I have cultivated both professional connections and meaningful friendships.
KM: The collaborative multidisciplinary aspect of ABM has opened an entirely new dimension in my professional and personal life. I have developed a much more complex understanding of breast biology and pathophysiology than I ever knew as a breast surgeon alone. I also have learned a great deal about pediatrics and the peripartum care of women, including the mental health challenges many patients experience. I have been so fortunate to have multiple mentors in breastfeeding medicine from different specialties, and I continue to learn something new each day. I feel like I have completed a second residency in breastfeeding medicine!
Q: What lead you to identifying the topic you chose for the Protocol?
HJ: As a surgical resident who plans to practice breast surgery, I have a strong professional interest in the intersection between breast cancer and breastfeeding. Little is taught about lactation in medical school or surgical training, yet breast surgeons and other physicians are entrusted with caring for breastfeeding patients with a current or past history of breast cancer. As a moderator for Dr MILK, I read countless questions from other physicians about breast cancer screening, breast cancer treatment during breastfeeding, and breastfeeding among breast cancer survivors. My impression was that physicians across multiple specialties would benefit from a practical, evidence-based resource to utilize when caring for this unique patient population.
KM: Hyperlactation often results in complications that are surgical in nature – such as plugging, galactoceles, abscesses, and nipple conditions. We thought it would be helpful to outline a standard approach to decreasing milk production in these patients to reduce maternal and infant complications of hyperlactation. At the IABLE Ranch conference in 2019, we drafted this protocol and had great input from colleagues in different specialties who have practiced breastfeeding medicine in a variety of contexts.
The intersection of breastfeeding and breast cancer is a very challenging clinical scenario, and can be difficult for patients psychosocially as well. Because we receive so many questions regarding this topic, we wanted to outline standard, evidence-based guidelines for the care of these patients.
Q: What difficulties has COVID-19 and its side effects (both in medicine and practice) presented to the implementation of your protocol? Or conversely, are there aspects of the current pandemic that have assisted it in any ways?
HJ: In general, there have been many delays in routine cancer screening as a result of COVID-19, and sadly there has been an increase in the proportion of cancers which are advanced at presentation. Many institutions had to halt non-emergent surgeries in order to divert resources towards care for COVID-19 patients, creating the need to utilize neoadjuvant treatment for breast cancers that were otherwise appropriate for up-front surgical therapy.
KM: Both cancer surgery and the care of breastfeeding dyads is not elective, so I have continued to see a large majority of patients in person, using standard precautions. Telemedicine has allowed me to care for patients in other parts of our state, but there are significant limitations to evaluation via telemedicine. The protocols have been very useful to share with colleagues during this time.
Q: In your own life, what ways have you seen the pandemic change your daily working and life routines?
KM: Remote learning is a real challenge for children and families. We are very fortunate that my son meets state of California childcare guidelines for attending transitional kindergarten in person. I am incredibly thankful to his school and teachers for what they do. I’m concerned about the multitude of psychosocial and economic impacts of the shutdown, as well as patients avoiding care for other medical problems not related to Covid.
Q: What are suggestions or tips you may have for physicians trying to implement your protocol, or more generally, support a breastfeeding parent at this time?
HJ: I would remind readers that these protocols are living documents which are updated regularly, and that there remain many areas in breastfeeding medicine with limited evidence. As such, I would encourage cross-disciplinary collaboration with other ABM members when seeking assistance for a challenging case as there may be more recent evidence to consider, and tips to be learned from the experiences of other breastfeeding medicine physicians.
KM: Using standard precautions, I think it’s essential to evaluate patients in person whenever safely possible.
Q: Any additional thoughts?
HJ: I would encourage surgeons who perform breast surgery to utilize ABM protocols and seriously consider joining ABM and learning more about breastfeeding medicine.
KM: Thank you to my ABM colleagues for their mentorship, friendship, and support. Thank you to Helen Johnson for her friendship and incredible work ethic as a researcher and publisher.
New Protocol on Breast Cancer and Breastfeeding
New Rochelle, NY, June 10, 2020 — Managing women with breast cancer who are breastfeeding is a complex issue. The Academy of Breastfeeding Medicine presents new recommendations in the peer-reviewed journal Breastfeeding Medicine. Click here to read the article now.
“The aim of this new protocol is to guide clinicians in the delivery of optimal care of breastfeeding women as it relates to breast cancer, from screening to diagnosis, treatment, and survivorship,” state coauthors Helen Johnson, MD and Katrina Mitchell, MD.
It addresses the spectrum of care, including oncologic breast surgery, chemotherapy, and adjuvant and endocrine therapy. A section on breastfeeding women who have a previous history of breast cancer is included.
Arthur I. Eidelman, MD, Editor-in-Chief of Breastfeeding Medicine, states: “This protocol is a guide for mothers who are undergoing diagnosis and treatment for breast cancer. It emphasizes that they do not have to categorically give up on their nurturing role as breastfeeding moms.”
Breast cancer is the most common malignancy in women worldwide. One in 20 women will develop breast cancer in their lifetime.
About the Journal
Breastfeeding Medicine, the official journal of the Academy of Breastfeeding Medicine, is an authoritative, peer-reviewed, multidisciplinary journal published 12 times per year in print and online. The Journal publishes original scientific papers, reviews, and case studies on a broad spectrum of topics in lactation medicine. It presents evidence-based research advances and explores the immediate and long-term outcomes of breastfeeding, including the epidemiologic, physiologic, and psychological benefits of breastfeeding. Tables of content and a sample issue may be viewed on the Breastfeeding Medicine website.
About the Academy of Breastfeeding Medicine
The Academy of Breastfeeding Medicine (ABM) is a worldwide organization of medical doctors dedicated to the promotion, protection, and support of breastfeeding. Our mission is to unite members of the various medical specialties with this common purpose. For more than 20 years, ABM has been bringing doctors together to provide evidence-based solutions to the challenges facing breastfeeding across the globe. A vast body of research has demonstrated significant nutritional, physiological, and psychological benefits for both mothers and children that last well beyond infancy. But while breastfeeding is the foundation of a lifetime of health and well-being, clinical practice lags behind scientific evidence. By building on our legacy of research into this field and sharing it with the broader medical community, we can overcome barriers, influence health policies, and change behaviors.
About the Publisher
Mary Ann Liebert, Inc., publishers is known for establishing authoritative peer-reviewed journals in many promising areas of science and biomedical research. A complete list of the firm’s 90 journals, books, and newsmagazines is available on the Mary Ann Liebert, Inc., publisher’s website.
Pregnant and Lactating Women with COVID-19: Scant Clinical Research
New Rochelle, NY, May 18, 2020 — Pregnant and breastfeeding women have been excluded from clinical trials of drugs to treat COVID-19, and as result, there is no safety data to inform clinical decisions. Such drugs include remdesivir according to a new article in the peer-reviewed journal Breastfeeding Medicine. Click here to read the article.
Since pregnant and lactating women are not included in clinical trials, little is known about whether the drug transfers into breast milk and reaches the infant’s circulation.
The lack of such data complicates a decision between giving lactating women a potentially life-saving drug and having them stop breastfeeding or risking any potential adverse effects of the drug on the infant, writes Alison Stuebe, MD, University of North Carolina School of Medicine and President of the Academy of Breastfeeding Medicine.
Suspending breastfeeding in mothers infected with COVID-19 could be detrimental because the infant is missing out on critical nutrients in human milk. Additionally, antibodies acquired from the mother may protect the infant against acquiring COVID-19.
“This quandary illustrates the consequences of longstanding policies to exclude pregnant and lactating women from clinical trials,” Stuebe says. “Rather than excluding pregnant and lactating women from research, we must protect them through research.”
Arthur I. Eidelman, MD, Editor-in-Chief of Breastfeeding Medicine, states: “Pregnant and breastfeeding women and their fetuses and infants cannot continue to be administrative orphans regarding new drug trials, and this situation warrants immediate correction.”
About the Journal
Breastfeeding Medicine, the official journal of the Academy of Breastfeeding Medicine, is an authoritative, peer-reviewed, multidisciplinary journal published 12 times per year in print and online. The Journal publishes original scientific papers, reviews, and case studies on a broad spectrum of topics in lactation medicine. It presents evidence-based research advances and explores the immediate and long-term outcomes of breastfeeding, including the epidemiologic, physiologic, and psychological benefits of breastfeeding. Tables of content and a sample issue may be viewed on the Breastfeeding Medicine website.
About the Academy of Breastfeeding Medicine
The Academy of Breastfeeding Medicine (ABM) is a worldwide organization of medical doctors dedicated to the promotion, protection, and support of breastfeeding. Our mission is to unite members of the various medical specialties with this common purpose. For more than 20 years, ABM has been bringing doctors together to provide evidence-based solutions to the challenges facing breastfeeding across the globe. A vast body of research has demonstrated significant nutritional, physiological, and psychological benefits for both mothers and children that last well beyond infancy. But while breastfeeding is the foundation of a lifetime of health and well-being, clinical practice lags behind scientific evidence. By building on our legacy of research into this field and sharing it with the broader medical community, we can overcome barriers, influence health policies, and change behaviors.
About the Publisher
Mary Ann Liebert, Inc., publishers is known for establishing authoritative peer-reviewed journals in many promising areas of science and biomedical research. A complete list of the firm’s 90 journals, books, and newsmagazines is available on the Mary Ann Liebert, Inc., publisher’s website.
Should infants be separated from COVID-19-positive mothers?
MARY ANN LIEBERT, INC./GENETIC ENGINEERING NEWS
New Rochelle, NY, April 9, 2020–In a new commentary, Alison Stuebe, MD, President of the Academy of Breastfeeding Medicine, addresses the risks and benefits of separating infants from COVID-19-positive mothers following birth. Although multiple public health organizations recommended keeping mothers and infants together, the United States’ Centers for Disease Control and Prevention advises facilities to consider separating mothers and babies temporarily until the mother is no longer contagious, and recommends that the risks and benefits of temporary separation should be discussed with the mother by the healthcare team.
In her commentary, Dr. Stuebe, Professor of Obstetrics and Gynecology at the University of North Carolina School of Medicine and distinguished professor in infant and young child feeding at the Carolina Global Breastfeeding Institute at the UNC Gillings School of Global Public Health, notes that there is no evidence to show that early separation of infants and mothers with suspected or confirmed COVID-19 improves outcomes. While separation may minimize the risk of transmission of the virus from mother to infant during the hospital stay, it has potential negative consequences for both mother and infant, according to the commentary published in Breastfeeding Medicine, the official journal of the Academy of Breastfeeding Medicine published by Mary Ann Liebert, Inc., publishers. Click here to read the protocol free on the Breastfeeding Medicine website.
Dr. Stuebe outlines several risks of separating mothers and infants in the hospital, which disrupts breastfeeding and skin-to-skin contact during the critical hours and days following birth. For example, infants who lack skin-to-skin contact with their mothers tend to have higher heart rates and respiratory rates and lower glucose levels. The separation also stresses the mother, which could make it more difficult for her to fight off the viral infection. In addition, separation interferes with the provision of maternal milk to the infant, which is important for the development of the infant’s immune system. Separation also disrupts breastfeeding, which puts the infant at increased risk of severe respiratory infections, including pneumonia and COVID-19.
“As we navigate the COVID-19 pandemic,” Stuebe writes, “I am hopeful that we can center mothers and babies and remember to first do no harm.”
Arthur I. Eidelman, MD, Editor-in-Chief of Breastfeeding Medicine, concurs that “there is no need or indication to categorically separate infants from COVID-19 suspect or positive mothers other than in circumstances wherein the mother’s medical condition precludes her caring for the infant. Feeding mothers’ own breast milk, either by nursing or by feeding of expressed milk, is OK and desired!”
About the Journal
Breastfeeding Medicine, the official journal of the Academy of Breastfeeding Medicine, is an authoritative, peer-reviewed, multidisciplinary journal published 10 times per year in print and online. The Journal publishes original scientific papers, reviews, and case studies on a broad spectrum of topics in lactation medicine. It presents evidence-based research advances and explores the immediate and long-term outcomes of breastfeeding, including the epidemiologic, physiologic, and psychological benefits of breastfeeding. Tables of content and a sample issue may be viewed on the Breastfeeding Medicine website.
About the Academy of Breastfeeding Medicine
The Academy of Breastfeeding Medicine (ABM) is a worldwide organization of medical doctors dedicated to the promotion, protection, and support of breastfeeding. Our mission is to unite members of the various medical specialties with this common purpose. For more than 20 years, ABM has been bringing doctors together to provide evidence-based solutions to the challenges facing breastfeeding across the globe. A vast body of research has demonstrated significant nutritional, physiological, and psychological benefits for both mothers and children that last well beyond infancy. But while breastfeeding is the foundation of a lifetime of health and well-being, clinical practice lags behind scientific evidence. By building on our legacy of research into this field and sharing it with the broader medical community, we can overcome barriers, influence health policies, and change behaviors.
About the Publisher
Mary Ann Liebert, Inc., publishers is a privately held, fully integrated media company known for establishing authoritative peer-reviewed journals in many promising areas of science and biomedical research, including Journal of Women’s Health, Childhood Obesity, and Pediatric Allergy, Immunology, and Pulmonology. Its biotechnology trade magazine, GEN (Genetic Engineering & Biotechnology News) was the first in its field and is today the industry’s most widely read publication worldwide. A complete list of the firm’s 90 journals, books, and newsmagazines is available on the Mary Ann Liebert, Inc., publisher’s website.
Academy of Breastfeeding Medicine Publishes New Bedsharing Guidelines
By Melissa Bartick, MD, MSc, FABM
The Academy of Breastfeeding Medicine has released its updated Bedsharing and Breastfeeding Protocol. The protocol presents evidence-based recommendations synthesized by an international collaboration of authorities on the topic who conducted a rigorous review of the literature.
Aimed at physicians and other health care professionals caring for families who have initiated breastfeeding, the protocol recognizes that bedsharing promotes breastfeeding. In contrast to recommendations by some organizations, breastfeeding mothers and infants are not advised against bedsharing, as long as no hazardous circumstances exist. The protocol emphasizes that all parents should be educated on safe bedsharing, recognizing that bedsharing is very common, and when bedsharing is unplanned, it carries a higher risk of infant death than planned bedsharing.
Hazardous circumstances include sleeping with an adult on a sofa or armchair; sleeping next to an adult impaired by alcohol, medications, or illicit drugs; tobacco exposure; preterm birth; and never having initiated breastfeeding.
The ABM protocol takes a “risk minimization” approach, emphasizing a discussion of risks and benefits of bedsharing with parents. This type of approach is being increasingly adopted in countries such as the UK and Australia. “Having conversations about safe bedsharing is important for removing stigma around the topic and facilitating open and honest dialogue between parents and providers,” says Dr. Lori Feldman-Winter, Professor of Pediatrics at Cooper Medical School in Camden, New Jersey and one of protocol’s authors. Dr. Feldman-Winter serves as co-faculty chair on the National Action Partnership to Promote Safe Sleep (US), and she was also an author of the American Academy of Pediatrics’ 2016 protocol on safe sleep.
ABM was pleased and honored to collaborate with three of the world’s leading experts on this topic: anthropologists Helen Ball and James McKenna, and epidemiologist Peter Blair. Dr. Blair, Professor of Epidemiology and Biostatistics at the University of Bristol (UK) is chair of the International Society for the Study and Prevention of Perinatal and Infant Death (ISPID), and Dr. Ball, Professor of Anthropology at the University of Durham (UK), directs the Durham Infancy & Sleep Centre, as well as serving on ISPID Board. Dr. McKenna is known for his ground-breaking work from his Mother-Infant Sleep Lab at the University of Notre Dame (Indiana, USA). Dr. Kathleen Marinelli, Clinical Professor of Pediatrics at University of Connecticut Medical Center and co-author, was instrumental in arranging the participation of Drs. Blair, Ball and McKenna.
In creating the protocol, we rigorously reviewed all available evidence about risk. In addition, we put the current research and evidence into historical context, noting that solitary sleep and artificial feeding are related and were recent developments in human history. We noted that some marginalized and low-income populations have a higher rate of sudden infant death as well as a higher rate of artificial feeding, thus measures to increase breastfeeding and lower the exposure to hazardous circumstances in these populations are important.
“The welcome fall in unexpected deaths over recent decades has come about through risk reduction advice being closely aligned to the available published evidence. This protocol takes the same approach,” says Dr. Blair.
Breastfeeding is important for safe infant sleep when bedsharing. “When bedsharing next to their mothers, breastfeeding infants sleep on their backs, and are naturally positioned away from pillows and objects that might obstruct their airways. Breastfeeding mothers form a protective position around their infant,” says Dr. Ball. Dr. Ball’s team provides detailed information for families through the Baby Sleep Information Source.
“Breastfeeding while bedsharing comprises a unique set of behaviors between mother and infant known as ‘breastsleeping,’ which also results in increased time breastfeeding compared to separate sleep,” notes Dr. McKenna. Breastfeeding is associated with a lower risk of Sudden Infant Death Syndrome.
As the person charged with seeing the protocol through to fruition from writing to approval, I found the process of achieving consensus on the evidence and recommendations to be both challenging and rewarding. It required working closely with many people who held a variety of differing viewpoints and experiences on the topic and finding common ground. We are thus especially satisfied that this protocol represents the best evidence-based and practical recommendations for clinicians. We hope this protocol will be widely used.
Melissa Bartick, MD, MSc is an internist at Cambridge Health Alliance and Assistant Professor at Harvard Medical School.
Posts on this blog reflect the opinions of individual ABM members, not the organization as a whole.
Team-based primary care breastfeeding support

(left to right) Samantha Walters IBCLC , Ann Witt, MD, IBCLC, Lauren Lasko APRN, IBCLC, Kristen Auletta, RN, IBCLC, and Maya Bolman, RN, IBCLC team-up and provide breastfeeding support.
Imagine seeing a breastfeeding family two days after hospital discharge and having the time needed to correct latch, help manage engorgement, or review hand expression and supplementation for the baby with poor weight gain. Health care provider support improves breastfeeding initiation and duration. Yet, too often primary care providers (PCP) do not have the time or knowledge to provide breastfeeding support after hospital discharge. These challenges can be solved with team-based lactation consultant and primary care (LC/PCP) providing breastfeeding support in the primary care office.
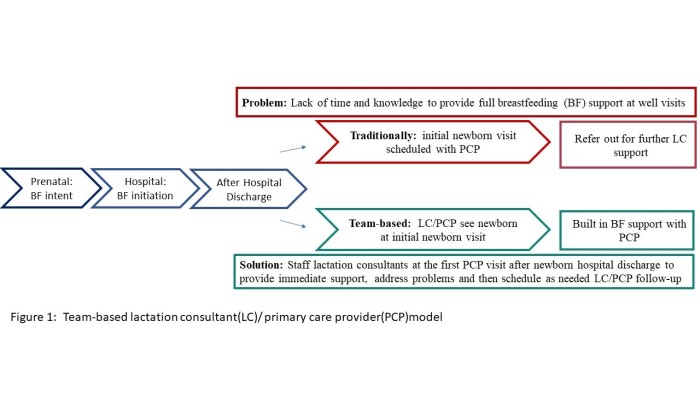
Per American Academy of Pediatrics and Family Physicians, a breastfeeding infant should be seen by their primary care provider (PCP) within two to three days of discharge (https://pediatrics.aappublications.org/content/125/2/405). This visit includes evaluation of weight and jaundice. In a breastfeeding infant, significant weight loss or jaundice is often triggered by breastfeeding difficulties including latch, pain, or delayed onset of milk production. Team-based primary care breastfeeding support combines the PCP’s initial post-discharge visit with lactation consultant support. The team approach facilitates physician evaluation of the infant along with immediate lactation support on needed topics such as feeding patterns, output, latch, engorgement, and appropriate supplementation.
Team-based LC/PCP care acknowledges:
- Families want to breastfeed.
- Families experience breastfeeding challenges.
- Feeding challenges require a plan that supports the breastfeeding dyad.
- Education on that plan takes time and breastfeeding knowledge.
Over 80% of mothers initiate breastfeeding in the United States, yet many women do not meet their goal of continued breastfeeding beyond a year. Given pain and low milk supply are common causes for weaning, breastfeeding support after hospital discharge is critical.

Ann Witt, MD, IBCLC, and Maya Bolman, RN, IBCLC with breastfeeding family during a clinic visit.
Having successfully provided team-based lactation care for over a decade within a suburban pediatric (https://www.ncbi.nlm.nih.gov/pubmed/21657890) practice, we look toward sharing this movement in other communities. Recently we partnered with a Federally Qualified Health Care system in Cleveland, Ohio to implement team-based lactation care.( https://www.jabfm.org/content/32/6/818) Prior to implementation a survey of providers at the FQHC found that 80% noted there was “not enough time” to provide lactation support during the visit and 58% thought there was “inadequate lactation consultant staffing at the practice” with 80% of PCP’s commenting that patients were “not receiving adequate help.” One year later, following implementation of team-based breastfeeding support, a repeat survey of PCP’s, found 100% reporting they were “providing better breastfeeding support” to their patients and liked having “breastfeeding support available for patient that NP/MD previously did not have time to provide.” A majority of the PCP’s also liked having “a lactation consultant join an already scheduled visit so the patient does not need an extra visit,” as well as “on-site immediate lactation support.” The program has been so successful that the FQHC is expanding this service beyond their main clinic to satellite sites.
To implement team-based care, practices need to personalize it to fit their own practice needs. We determined feasibility of the team-based practice model at the FQHC by assessing breastfeeding intent and rates, health care provider knowledge, billing reimbursement, and currently available breastfeeding supports. We used the information gathered to formulate a business plan, identify additional training needs, and facilitate communication with administration. Other practices can build on this structure to implement team-based LC/PCP care in their own communities.
Now is the time for our health care system to help families get timely breastfeeding support after hospital discharge. If your practice has already implemented a team-based primary and lactation care approach share your story so others know it is possible. If you are interested and trying to figure out how, gather the basic information, begin the dialogue and draw on other practice’s experience.
Together we can improve the care of our families after delivery, and better support breastfeeding duration!
References:
- Stark et al. Committee on Fetus and Newborns 2008-09. Hospital Stay for Healthy Newborns. Pediatrics February 2010, 125 (2) 405-409;
- Witt AM1, Smith S, Mason MJ, Flocke SA. Integrating routine lactationconsultant support into a pediatric practice. Breastfeed Med. 2012 Feb;7(1):38-42.
- Witt AM, Witt R, Lasko L, Flocke SA Translating Team-Based Breastfeeding Support into Primary Care Practice. JABFM Nov/Dec 2019
Blog posts reflect the opinions of individual authors, not ABM as a whole.
Baby Friendly Increases Breastfeeding Rates— The Problem with the Fancy Graph Study
By Melissa Bartick, MD, MSc, FABM
Did the Baby-Friendly Hospital Initiative meet its intended goal of increasing breastfeeding across the United States? A recent study claims it failed. The study, published in The Journal of Pediatrics by Bass and colleagues, is replete with fancy statistics and graphs, but the obvious answer is that Baby-Friendly is succeeding. Anyone interested in breastfeeding knows that breastfeeding rates across the US have risen as the percentage of births in Baby-Friendly Hospitals has risen. Study after study, including a meta-analysis, have shown the efficacy of the Baby-Friendly Hospital Initiative (BFHI) in increasing breastfeeding rates and improving health outcomes. Furthermore, other studies have shown that the Ten Steps have additive effects in increasing breastfeeding rates.
The problem with the study by Bass and colleagues is that it compared breastfeeding rates among all US states and the percentage of births in Baby-Friendly hospitals among all US states at a single recent point in time. And, not surprisingly, there was no correlation between breastfeeding rates in the different states and the percentage of Baby-Friendly births. Why? For two reasons. First, the very best way to look for the effect of an intervention is with a randomized control trial. This was done with Baby-Friendly in the PROBIT trial, which found that 3 month exclusive breastfeeding rates were 6% in the hospitals without the intervention compared to 43% with implementation of a BFHI-type intervention. If such a trial isn’t possible, the best way to judge the efficacy of an intervention is to look at the outcomes over time as the intervention is implemented. That way, one can infer cause and effect.
The other reason why the study’s conclusions aren’t valid is that states can have markedly different baseline breastfeeding rates due to a variety of socio-demographic factors, like education, income, and culture. For example, even before there were many Baby-Friendly Hospitals, Louisiana and Vermont had very different breastfeeding rates. So, course, if you compare their breastfeeding rates to each other as a function of Baby-Friendly, the result will look like nonsense. You can only compare a state to itself over time as Baby-Friendly is implemented. Or you can look at the entire US over time as a function of Baby-Friendly implementation. But you can’t compare Louisiana to Vermont at the same time, which is what these authors did.
As far as the Bass study goes, the authors claimed they tried to minimize a type of bias known as ecological fallacy by controlling for each state’s birth rate. But breastfeeding rates are unaffected by birth rates. It is commonly known that breastfeeding rates are highly affected by sociodemographic factors, yet the authors made no attempt to control for these factors. The CDC reports breastfeeding rates by racial and ethnic groups, and their data shows different racial and ethnic groups have markedly different breastfeeding rates, and we know the populations of different racial and ethnic groups are not evenly distributed among the states. Their study reports sophisticated statistical methods and shows complex figures, complete with mathematical formulae, which gives their study the appearance of professorial authority. Unless one has an advanced degree in biostatistics, the way their methods and findings are displayed may be difficult for most readers to understand. Readers may even fail to notice that the basic premise of their methods is so flawed that the study should have never been performed, let alone published. It is the intellectual equivalence of the “The Emperor Has No Clothes.” The efficacy of an intervention simply cannot be ascertained by looking at one point in time and across populations that are highly diverse.
Here are some statistics to dig deeper, taken from the CDC’s Breastfeeding Report Cards:
In 2007, only 1.8% of US births occurred in Baby-Friendly Hospitals and the US breastfeeding initiation rate was 75% with a 3-month exclusive breastfeeding rate of 33%. Yet in 2016, 18.3% of US births occurred in Baby-Friendly hospitals and the 2015 initiation rate grew to 83.2% and with a 3-month exclusive rate of 46.9%. As individual hospitals become Baby-Friendly, they see their exclusive breastfeeding rates at discharge increase markedly. Achieving certain exclusive breastfeeding rates at discharge is even part of the criteria for becoming a Baby-Friendly hospital, so we know on a micro level that Baby-Friendly increases breastfeeding rates.
For example, in 2004, Louisiana had 0 Baby-Friendly hospitals and a 56.6% initiation rate with an exclusive breastfeeding rate 22.0% at 3 months. By 2016, 12.7% of births occurred in Baby-Friendly facilities, which would leap to 41% in 2018, related to work from the CHAMPS initiative. By 2015, Louisiana’s breastfeeding initiation rate grew to 67% and it’s 3 month exclusive rate grew to 39.6%.
Vermont, by contrast, had an 85.2% breastfeeding initiation rate and 47.3% exclusive breastfeeding at 3 months in 2004, much higher than the national average. By 2015, was at 89.3% and 62.8%. Vermont had 3.8% of births occur in Baby-Friendly facilities in 2004, and this went up to only 10% in 2015.
Vermont was starting the breastfeeding race way ahead of Louisiana when Baby-Friendly came in, so a recent snapshot comparing their breastfeeding rates and Baby-Friendly births is meaningless. In Vermont, breastfeeding has been a normal part of the culture, whereas breastfeeding has historically been seen as unusual in Louisiana. Louisiana has also consistently ranked among the lowest states in household income and education, while Vermont has consistently been ranked as one of the highest.
Vermont’s relatively wealthy, well-educated population may be predisposed to breastfeed at increasing rates over time, despite not having formal Baby-Friendly designation at 90% of its hospitals. If we only look these states from the current snapshot in time, Louisiana has higher Baby-Friendly “penetrance” with lower breastfeeding rates than Vermont, and we miss the likely impact of Baby-Friendly on that state. In addition, research shows that Baby-Friendly is important for reducing racial disparities in breastfeeding the Southeastern US.
Multiple previous studies have demonstrated the efficacy of the Baby-Friendly Hospital Initiative and the Ten Steps. Those studies still hold more power than one poorly done study with some fancy graphs.
Blog posts reflect the opinions of individual authors, not ABM as a whole.
###
Towards Improved Support for Medical Trainees Who Are Breastfeeding
Dr. Helen Johnson
Ironically, physicians have some of the lowest rates of breastfeeding in the United States. Despite acute awareness of the medical risks of not breastfeeding and deep commitment to educating their patients about the importance of breastfeeding, many physician mothers face significant challenges in their own breastfeeding efforts. Medical trainees – including medical students, resident physicians, and fellows – are among the most vulnerable. This month’s IABLE podcast focuses on how to improve support of medical trainees who are breastfeeding.

Medical trainees have jam-packed schedules with little to no control over their time. It can be a small feat to find time to scarf down a snack between surgeries or surreptitiously slip away from hospital rounds to run to the bathroom. In a culture in which self-sacrifice for the greater good of one’s patients is the norm, devoting 20-30 minutes every few hours to express breastmilk can feel like an indulgence. In addition, trainees may fear being perceived as less dedicated than their peers to their education or to patient care should they attend to personal needs at work. Even in a workplace environment that strongly supports breastfeeding – such as the obstetrics/gynecology department – lack of accessible, sanitary, and private spaces can limit a trainee’s ability to breastfeed at work.
In the past several months, several steps have been taken to improve support for medical trainees who are breastfeeding. In June, the American Academy of Family Physicians (AAFP) published a statement (https://www.aafp.org/about/policies/all/breastfeeding-accommodations-trainees.html) stressing the need to better support these women through policies that address protected time, adequate facilities, and a supportive workplace environment. On July 1, new Accreditation Council for Graduate Medical Education (ACGME) regulations went into effect: residency and fellowship programs are now required to provide clean, private lactation facilities for trainees that are in close proximity to patient care and include refrigeration capabilities.
The ACGME notes: “While space is important, the time required for lactation is also critical for the wellbeing of the resident and the resident’s family.” Last month, a departmental lactation policy implemented by the surgery departments at the University of Michigan and the University of Wisconsin was published. This policy has been circulated on social media and adapted by dozens of other departments across the nation.
Most recently, my colleagues and I issued a “call to action”, urging the creation of a universal policy to better support resident physicians and fellows who are breastfeeding. We admire the grassroots efforts to create departmental policies and respect the significance of the new ACGME regulations. However, we feel that there is an urgent need to do more to ensure that all medical trainees have the support they need to breastfeed their children. In our publication, we underscore the importance of cultivating a supportive workplace culture, promoting access to appropriate lactation spaces, and ensuring adequate time for breastfeeding, and suggest specific action steps that program directors and institutional leadership can take to achieve these goals. Our piece was highlighted by Duke Forge and is discussed in detail in this month’s IABLE podcast.

The podcast features not only the three authors of the “call to action” but also Laurie B. Jones, the founder of Doctor Mothers Interested in Lactation Knowledge. This online peer-to-peer breastfeeding support group for physician mothers has been instrumental in helping thousands of women – including trainees – meet their breastfeeding goals. Dr. MILK members encourage each other and share their wisdom for balancing breastfeeding and a medical career. Let’s take this to the next level by joining forces with breastfeeding medicine physicians and national organizations – together, let’s advocate for a universal lactation policy for medical trainees. ABM has already confirmed their support of the AAFP’s statement. Now it is time to amplify each other’s voices and effect meaningful change.

– Helen M. Johnson, MD is a general surgery resident at East Carolina University / Vidant Medical Center in Greenville, North Carolina. She is originally from Tampa, Florida and obtained her medical degree from the Warren Alpert Medical School of Brown University. Dr. Johnson plans to pursue fellowship training in breast surgical oncology after graduation from residency. She has a special interest in the intersection of breast cancer and breastfeeding, and is working towards IBCLC certification. Dr. Johnson enjoys gardening, playing the cello, and spending time with her husband, two children, and beloved cat. Connect with Dr. Johnson on Twitter: @HelenMJohnsonMD
Blog posts reflect the opinions of individual authors, not ABM as a whole.
First Droplets Website: Empower Parents Enable Breastfeeding #WBW2019

By Dr. Jane Morton
“I’m going to try.” This is the tentative answer many mothers give, instead of “Yes, I’m going to breastfeed!”
Why do so many women worry that breastfeeding may be complicated, painful and probably dependent on professional help? If breastfeeding is so natural, why doesn’t it come naturally, as it seems to in all other mammals? Over the past several decades, research in human lactation steers us to the answers, pointing directly to the sensitive time in the first few hours immediately after delivery. What does or does not happen in this window may determine whether mothers give up on breastfeeding for problems related to, what could be called the ABC’s of breastfeeding. A = attachment (how a baby latches on and transfer milk from the breast), B = breastmilk production, and C = calories or what a baby consumes.

The longer the interval between birth and the first feed, the greater the likelihood a baby will have some issues with latching and comfortably removing milk, or “A = attachment”. Likewise, the longer the interval between birth and the early, (first hour) frequent and effective removal of milk, the weaker the signal to the breast to make milk (B = breastmilk production). This may compromise subsequent production potential. And finally, the more protracted the delay before the first feed, the greater the compromise of passive and active immunity, provided by the multitude of bioactive factors that enhance the functionality of the infant’s own immune system.
Weight loss differentials between infants who feed in the first hour, compared to those who do not, become evident as early as 6 hours. The “last supper” for the newborn ends after delivery with the cutting of the umbilical cord. So presumably, it’s not hunger that drives the newborn mammal to immediately seek out the breast, but a grand design, so to speak, to protect the cornerstones of breastfeeding.
Unlike other mammals, the “naturalness” of the human birth process has been challenged by surgery, drug and early gestation delivery. For example, cesarean delivery, induction and preterm births reduce the likelihood a baby will feed effectively in the first hour. That said, there are simple solutions to avoid complex problems, that become less remedial by the hour. It’s all about learning comfortable techniques and easy-to-remember facts about the ABC’s before D, delivery.
The goal of a new website, www.firstdroplets.com, is to give an expectant mother the tools she’ll need to protect her own breastfeeding experience, no matter what the delivery scenario. Counting down the days before delivery, she can anticipate the opportunities of the first hours. For breastfeeding to be fun, nursing needs to be comfortable for her and easy for her baby. And she needs to make plenty of milk. The short and simple lessons aim to prepare her to answer these questions:
1. What is a “good” latch and why is it important?
2. What do I do to help my baby with a latch, if needed?
3. How do I make more milk sooner?

Using props, animation and real mothers and babies in their 1st postpartum hours, expectant mothers learn about the magic of that first feed when things go “naturally”. To reduce her worries, she also learns that if there are any concerns, she can use the best and most “natural” tools, her hands, to help her baby and protect her production. Hand expression and feeding “dessert from a spoon” are normalized as the first hour response for the baby unable to latch. “Handling” breastfeeding includes suggestions on holding and positioning baby and breast for comfortable and effective nursing, not waiting for soreness to develop.
A separate video for a mother expecting a premature NICU baby aims to prepare her for the earliest challenges and give her a sense of control and recognition for the vital role she’ll play in continuing to protect her baby.
The website, videos, graphics, participant mothers and donations to fund this project were all inspired by the hope that new mothers and their partners come to delivery with confidence, answering “Yes, I’m going to breastfeed!” Please join our effort spreading the word.
Our thanks,
Jane Morton, MD
Website videos may be downloaded for educational non-commercial use. References to support the science behind the video are summarized in a website section and in a recent publication: Morton J. Hands-on or hands-off when first milk matters most? Breastfeeding Med. 2019;14(5):295-297.
Blog posts reflect the opinions of individual authors, not ABM as a whole.